Meet Our Keratoconus Specialist in Burlington, New Jersey

Dr. Lauren Rineer graduated with honors from New England College Of Optometry in 2018. She also received The Excellence in Vision Therapy Award in 2018. She practiced in New York where she honed her specialty in pediatric optometry and myopia management. Dr. Rineer also treats patients with various ocular conditions and diseases.
Dr. Luong received her Bachelor of Arts degree in Interdisciplinary Science from Arcadia University and earned her Optometry degree from Pennsylvania College of Optometry at Salus University in 2018. She achieved clinical honors during her externship rotations at this very practice in Burlington, NJ; Scranton, PA; Wilkes Barre, PA; and Miami, FL which all focused on primary care and ocular diseases. Dr. Luong is a member of both American Optometric Association and Pennsylvania Optometric Association. She is licensed to practice in both Pennsylvania and New Jersey.
What got you started with myopia management? And maybe you could share a little bit about how it became an interest and where you developed your expertise in it?
So I kind of got into it when I was in school and I heard about Ortho-k lenses. For the past seven years now, throughout the practice, I’ve been seeing a lot of kids at our office and everyone’s nearsightedness. So why don’t we bring this into the office and try to do eye drops? I mean, my major thing is doing ortho-k for the little ones because I feel like it’s actually helping. As an example, my prescription hasn’t changed at all. So I think that’s how I warmed up to the whole concept.
So you wear ortho-k lenses yourself? What’s been your experience with them?
Yes, I wear ortho-k lenses myself, and my experience has been great. No side effects, even though I wear them every single night. I’ve been fitting a few patients in them as well, and their experiences have been similar to mine. No issues so far. Their prescription hasn’t changed much so far, thanks to ortho-k..
Maybe you could share a little bit about the treatments you offer and how do they differ?
So we do atropine drops, which is the dilation drops for the younger crowd who can’t wear contacts yet, and that is to help control their accommodation throughout the day. Because of nearsightedness, essentially their prescription is fixed for far distance. But over time, because they’re wearing their glasses full time, they’re over-accommodating for their close-up activities at school. So the eye drops help combat this by relaxing accommodation, which will hopefully slow down changes that may cause myopia.
As the child gets older, we would move more toward soft contact lenses, or ortho-k for the ones who don’t want to wear contacts or glasses at all anymore. They can just sleep in the specialized rigid gas permeable ortho-k lenses at nighttime, and it’ll correct their vision as they sleep. They can simply wake up in the morning, and have clear vision without contacts or glasses.
Do you decide for the patient what myopia control method they want, or do they decide for themselves?
When deciding which method to go with, we lay out all of the options for them, and ask the patient to see what they’re comfortable with. This is especially true if they’re doing sports or similar activities. Some little ones are hesitant to try out contact. So we choose the best option for them based on what their prescription is, and what they’re most comfortable with. We never push something that the patient says they don’t want or aren’t interested in.
For patients who are interested in contacts, how do they decide between going with the multi focals or ortho-k?
There are a few factors. What activities are they involved in? Do they want to wear their contacts on a daily basis? Also, the patient’s prescription plays a role, because ortho-k only goes up to a certain prescription strength. Cost is often also a factor when deciding.
What do you think parents need to learn about myopia and the importance of myopia management?
They need to know that everyone’s on screens right now for way longer than is healthy, especially with the COVID pandemic. And that’s really harmful for everyone’s eyes.
Parents also need to know that myopia can take a toll on their child’s eyes that goes way beyond just not being able to see clearly from far away. The eyeball itself kind of grows as you age. So as your child becomes more nearsighted, their risk grows of developing eye diseases like glaucoma or cataracts. As the eye grows, the structures of the eye also stretch, so something like retinal detachment also becomes more likely as the eye gets elongated.
Myopia management prevents the eye from growing too quickly, minimizing the risk for disease.
How do you speak to parents and kids about myopia management? Do you talk to the parents first, or everyone at once?
I’m a visual person, so I kind of explain it in the same way it works in my head. So I use visual aids, and the parents will usually get it. And speaking to the kids, it’s just helping them see it’s important to wear their glasses by showing them what their vision is like without it.
I try to get the kids excited, make them feel empowered, like this will be great for everybody. Like with braces, for example, even though it’s a different industry, there’s a whole bunch of hesitation because you have to wear these things in your teeth. But in the end, you kind of know that it’s important. So for kids, it’s like they don’t want to do it, but they want to do it. It’s a very tough decision, but I find in eye care, it’s like the opposite. They often either want to wear glasses or they want to wear contacts. It’s always positive. It’s an interesting switch.
Is there anything that you feel that you’d like to add about my management that you’d like to maybe have us include on that section of the site?
I wish people could know more about myopia control, because every time I bring it up in the office, no one hears about it at all. So just kind of want to make it out there. That it’s been around for at least ten or twenty years already.

Dr. LaTorre received her Doctor of Optometry degree and BS in Vision Sciences from the Pennsylvania College of Optometry. She graduated Magna Cum Laude from Shippensburg University with a degree in Biology and was a member of the Biological honors society Beta Beta Beta. Dr. LaTorre received clinical honors throughout all of her clinical rotations which focused on ocular diseases such as anterior segment disease, glaucoma, diabetic retinopathy, and macular degeneration.

Dr. Julie Greenberg is an associate at Dr.'s Eyecare Center. After completing her undergraduate study in Nutrition and Biology at the University of Delaware in 2002, Dr. Greenberg received her Optometry degree from The Pennsylvania College of Optometry in 2006. She completed an externship at the San Diego Naval Medical Center during her studies at the Pennsylvania College of Optometry. Dr. Greenberg is a member of both the American Optometric Association and the New Jersey Society of Optometric Physicians. She has been licensed to practice in New Jersey since 2006.

Dr. Shetzline is an associate of Dr.'s Eyecare Center specializing in Geriatrics and Low Vision Rehabilitation. Dr. Shetzline completed his undergraduate study in Biology at Messiah College prior to receiving his Optometry degree from the Pennsylvania College of Optometry in 1998. Dr. Shetzline also completed an externship with the The Philadelphia Veteran's Medical Center during his studies at the Pennsylvania College of Optometry. In addition to his membership to the American Optometric Association, Dr. Shetzline has also been appointed as staff to various organizations including, the Burlington Woods Convalescent Center, the Granville Assisted Living Center, the Brendenwood Retirement Village, the Alterra Sterling House Assisted Living, the Alterra Clare Bridge Assisted Living, and Sunrise At Floral Vale Assisted Living.

Dr. Levy is the Chief Medical Director of Drs. Eyecare Center. After completing his undergraduate study in Biology at Temple University in 1989, Dr. Levy studied at the Pennsylvania College of Optometry where he received his Optometry degree in 1993. During his studies at the Pennsylvania College of Optometry, Dr. Levy completed an externship at the Delaware Veteran's Medical Center. In addition to his position as the Chief Medical Director at Dr.'s Eyecare Center, Dr. Levy has also served as LASIK Consultant at Kremer/TLC Laser Centers in Cherry Hill, NJ. Dr. Levy has been licensed to practice optometry in both New Jersey and Pennsylvania since 1993. He is a member of the American Optometric Association, the New Jersey Optometric Association and the West Jersey Optometric Association where he was appointed as Secretary. He has also been appointed as a Clinical Preceptor by the Pennsylvania College of Optometry (now Salus University).
Our Doctor Can Diagnosis and Treat Keratoconus
Your cornea is the transparent, outer lens of your eye, and it typically has a smooth dome shape. Keratoconus describes a condition in which the corneal structure isn’t strong enough to maintain a healthy ball shape.
Meet with our Keratoconus Specialist in Burlington, New Jersey to define your eye's condition and ways for treatment.
As a result, the cornea bulges outward into more of a cone. Our professional optometric team at our eye care clinic is knowledgeable about how to diagnose and treat keratoconus.
Keratoconus is rare, with an estimated one person out of every 2,000 having the condition. It generally appears in the teenage years and can progress slowly or rapidly.
Keratoconus also runs in families, so if you or your children are at risk, it’s advised to contact us for a thorough eye exam.
Causes of Keratoconus
Your cornea is held in place by very small collagen fibers. When they are weakened and too fragile, they aren’t able to preserve the round shape of your cornea.
A reduction in the protective antioxidants of your cornea, which act to destroy damaging by-products made naturally by corneal cells, is what causes keratoconus.
In addition to genetics, some types of eye injuries may increase your chance of being diagnosed with keratoconus.
Specific ocular diseases, such as retinitis pigmentosa, vernal keratoconjunctivitis and retinopathy of prematurity, as well as some systemic conditions (Down syndrome, Ehlers-Danlos syndrome, Leber's congenital amaurosis and osteogenesis imperfecta) are also associated with this corneal abnormality.
Our Keratoconus Specialist in Burlington, New Jersey has years of experience identifying the various levels of keratoconus and other corneal conditions.

Symptoms of Keratoconus
When the shape of your cornea begins to bulge, it alters your eyesight in two different ways. As the cone shape forms, your normally smooth corneal surface becomes wavy, called irregular astigmatism. Additionally, as your cornea expands, vision becomes increasingly nearsighted. Focusing becomes impossible without eyeglasses or contact lenses. Usually, the problems begin in one eye and develop later in the other eye too.
Typically, patient’s eyeglass prescription will change often as the vision becomes worse and contact lenses will be difficult to wear due to discomfort and improper fit.
When keratoconus become more severe (which usually takes a long time however on occasion can happen rather quickly), the cornea can begin to swell and form scar tissue. This scar tissue can result in even further visual distortion and blurred vision.
Altogether, these changes can create the following symptoms:
- Blurred vision
- Streaking of lights
- Halos around bright lights at night; glare
- Sudden change of vision in only one eye
- Objects appear distorted, both near and distant
- Double vision from just one eye
- Triple ghost images
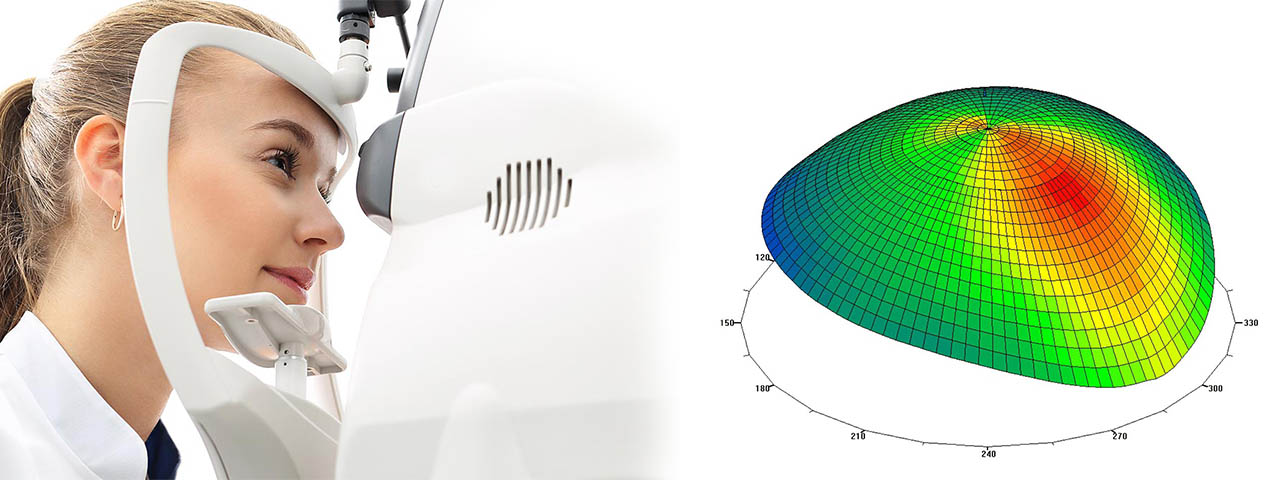
How We Diagnose Keratoconus
Our eye doctors will inspect carefully for the signs of keratoconus during your comprehensive eye exam. It’s critical to inform us of any symptoms that you’ve been experiencing. To diagnose the condition, we’ll measure the shape of your cornea. Computerized Corneal Topography is used for this procedure, which takes a picture of your cornea and analyzes it instantly.
